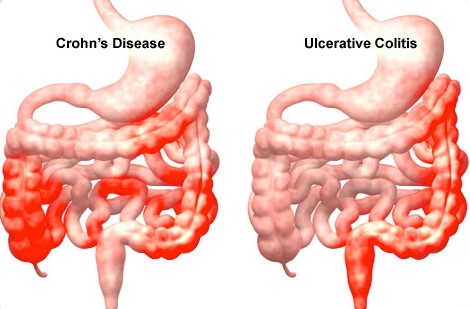
Inflammatory Bowel Disease (IBD) – Crohn’s & Ulcerative Colitis
Both Crohn’s and Ulcerative Colitis are known as inflammatory bowel disease (IBD). Different from IBS or irritable bowel syndrome, where the muscles contract abnormally. IBD refers to the chronic inflammation of the large intestine. It is the result of the body producing inflammation as it mistakes normal bacteria that travels along the GI tract, as a harmful virus, fungi and other foreign invaders. The body’s inflammatory response can cause ulcers to form on the intestines, resulting in the tissues to swell and eventually scar. The intestines eventually begin to narrow and stiffen, causing severe abdominal pain and a long list of digestive issues. As bacteria is ever present in the GI tract, this inflammatory response is continuous. Approximately 1.5 million people suffer from either of these diseases.
Similarities and Differences 
While both Crohn’s and Colitis can affect the large intestine, they are not completely equal. Inflammation triggered by Crohn’s disease can affect any area along the GI tract and can form in patches while Ulcerative Colitis affects only the large intestine (rectum and colon) and stretches through the entire affected area. The inflammation from Colitis, differs in that it is only present in the innermost lining of the colon.
What can cause IBD?
What causes IBD remains unclear however, studies have found individuals who engage in poor lifestyle habits such as smoking, consuming a poor diet, prolonged use of non-steroidal anti-inflammatory drugs such as ibuprofen or naproxen sodium found in Aleve, or who are under constant stress, are just some of the factors linked to the onset of IBD. Genetics plays a role as well as studies have shown up to 20 percent of individuals who have a sibling or parent affected by IBD, will develop it in the future.
Symptoms for both:
Diarrhea
Abdominal pain
Rectal Pain or bleeding
Blood in the stools
Weight loss
Fatigue
Fever
Perianal disease (inflammation near the anus) as well as irritation of the skin, eyes, joints, liver or bile ducts and sores in or around the mouth – Symptoms common in Crohn’s disease.
Dehydration- Symptom common in Ulcerative Colitis
Although chronic, IBD eventually goes into remission that can range from weeks to even years. As occasional flare-ups do happen, the frequency decreases dramatically through holistic treatment and consuming an anti-inflammatory diet as opposed to one that contributes to inflammation, provoking the symptoms.
What to eat
A diet made up primarily of alkalizing foods such as lean proteins and low-glycemic index foods. Which would be your dark leafy greens and vegetables, healthy fats like coconut oil, olive oil and avocado and foods high in omega-3s like flax seeds, walnuts, chia seeds and wild caught salmon. A balanced intake of each has been proven to significantly reduce inflammation as well as removing toxins from the body. 
The addition of supplements that promote a healthy gut and helps coat the lining of the digestive tract should be included in your diet as well. Probiotics, often referred to as the “good bacteria” are critical for your gut’s health as they aid mineral absorption and boost digestive function.
During a flare-up, tissue healing supplements like glutamine powder as well as an herb known as slippery elm are wonderful sources. Slippery elm or red elm is an herbal remedy containing mucilage and adapts a gel-like substance when mixed with water. Once ingested, it coats the mouth, throat, stomach and intestines, aiding in tissue repair and protects irritated tissue from further damage.
Anti-inflammatory supplements include fish oil, turmeric and curcumin, a component found in the turmeric root. These herbs have not only been a powerful tool used to combat joint pain but studies have shown their anti-inflammatory properties have led to a significant decrease in symptoms of IBD.
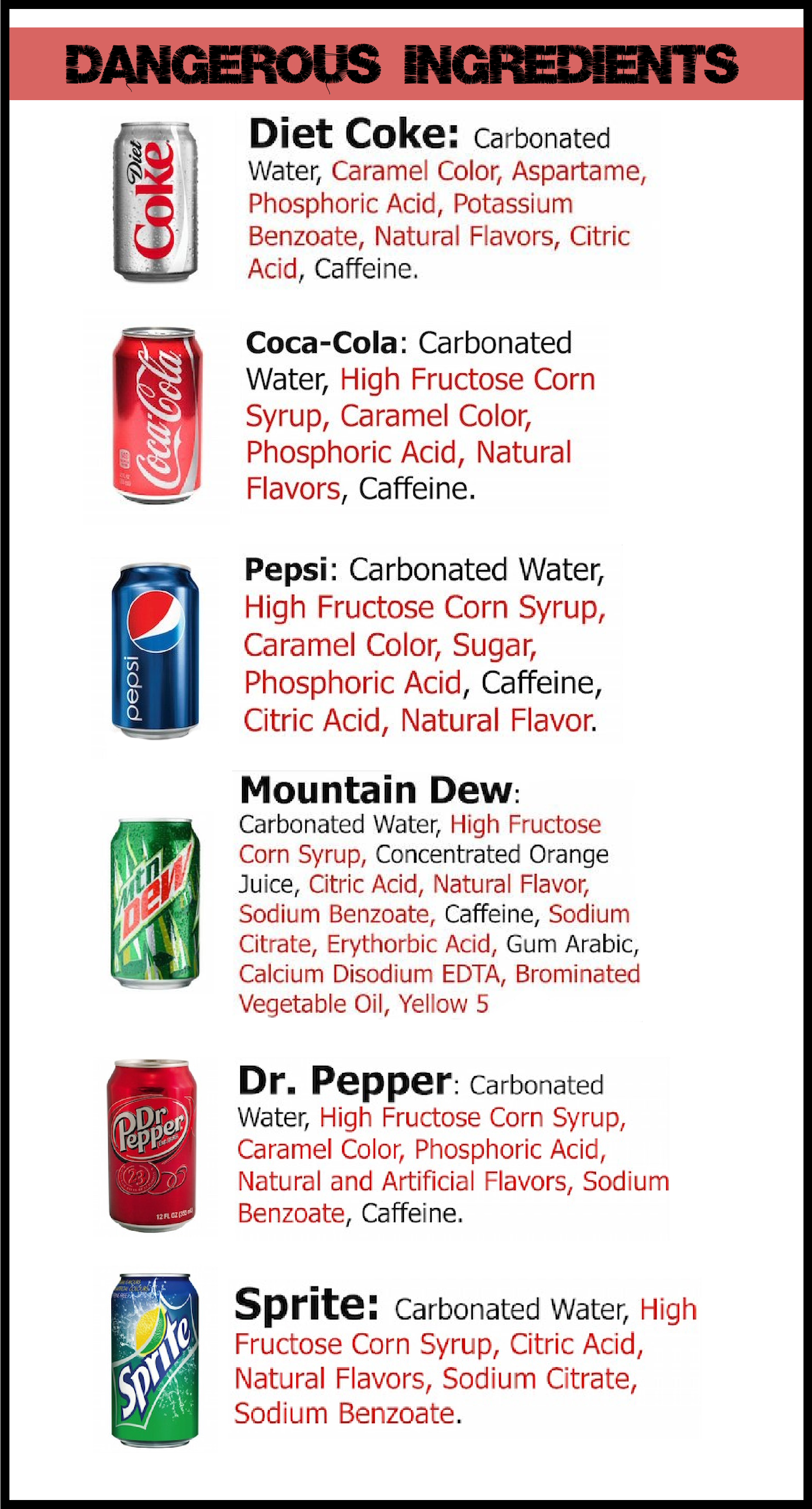
What to Avoid
Foods that should be avoided include foods with a high-glycemic index, such as white breads and pastas, refined sugar, alcohol, caffeine, carbonated drinks, dairy, gluten, spicy foods, or foods high in fiber.
Easy Changes
Stress can play a major factor in how your body manages IBD and potentially worsening the flare-ups. When stress is prevalent, the immune system weakens and inflammation increases. A stroll in the park, a bike ride or any favorite activity that gets your blood moving will help to ensure you are getting enough exercise and allowing yourself time to relax the best you can. 
Drinking plenty of fluids aid in digestion and prevents dehydration that is common symptom of Ulcerative Colitis.
Eating smaller meals that are easily digestible or consuming liquid meals such as smoothies or meal replacement shakes.
At Forum Health Clarkston let us share our expertise guiding you through how to stay in control of chronic inflammation and limit the severity of IBD flare-ups. We have helped clients adopt an appropriate nutrition plan and lifestyle changes leading to healing from the inside. Let us customize a plan for you.
Forum Health Clarkston
248-625-5143
References
Axe, Josh. (2015, August 28). Ulcerative Colits Diet. Retrieved from:
https://draxe.com/ulcerative-colitis-diet/
Axe, Josh. (2016, February 16). Crohn’s Disease Diet. Retrieved from:
https://draxe.com/crohns-disease-diet/
Daller, John. (2016, May 3). Crohn’s Disease Causes, Symptoms, Diet. Retrieved from:
http://www.onhealth.com/content/1/crohns_disease
What is Crohn’s Disease. Retrieved from:
http://www.crohnscolitisfoundation.org/what-are-crohns-and-colitis/what-is-crohns-disease/